Painful periods and Endometriosis
Did you know? Anti-inflammatories from the drug store (ibuprofen or naproxen) can reduce pain and period flow by up to 50%. Minimize stomach upset by taking with food.
Pelvic floor physiotherapy to relax the pelvic floor tension can help with pain. Local heat, TENS, acupuncture, and exercise have proven benefits. Vitamin B complex, ginger, and fish have been shown to decrease menstrual pain.
Painful periods (dysmenorrhea) can be caused by
inflammation hormones (prostaglandins) and cramps
heavy periods (uterus cramps to stop the bleeding)
endometriosis (when uterine lining-like tissue grows outside the uterus into the pelvis or abdomen)
adenomyosis (when the uterine lining grows into the uterine wall); bulky uterus. This condition can also be seen on imaging but have no symptoms.
abnormal ovarian cysts (not the physiological normal ones we make monthly that release the egg)
infections, such as pelvic inflammatory disease
structural factors such as fibroids or abnormal anatomy
copper IUD in some people
Dr. KIrkham on painful periods (text) or video WCH Matters
Endometriosis info from yourperiod.ca SOGC
INFOGRAPHICS
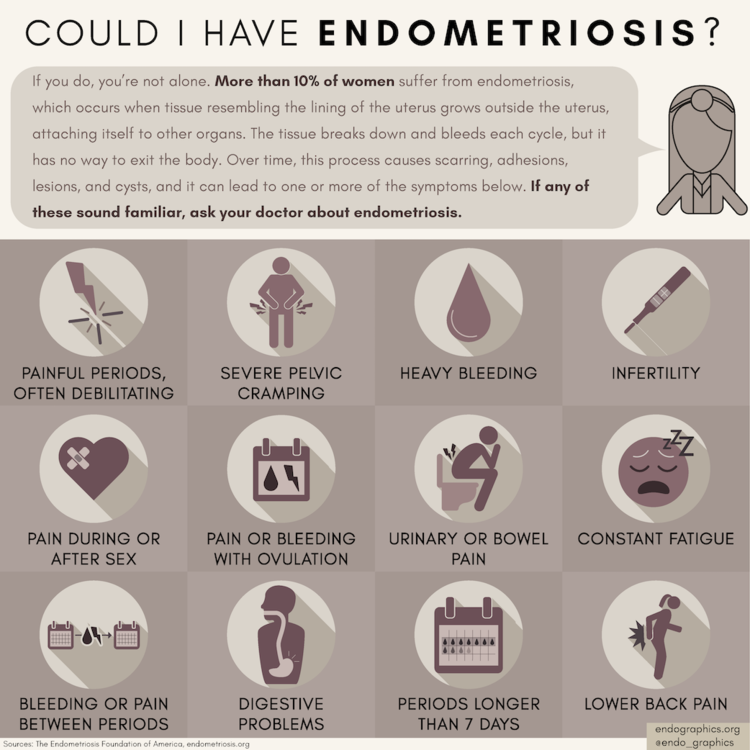
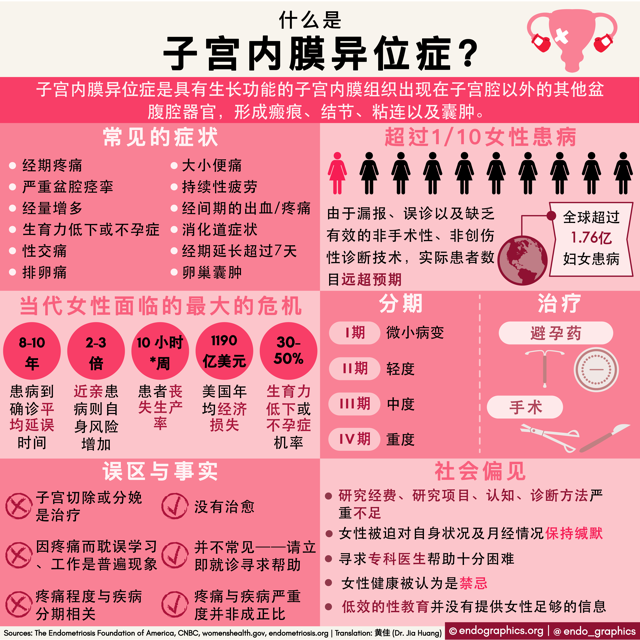
English and Spanish Infographics from endographics.org
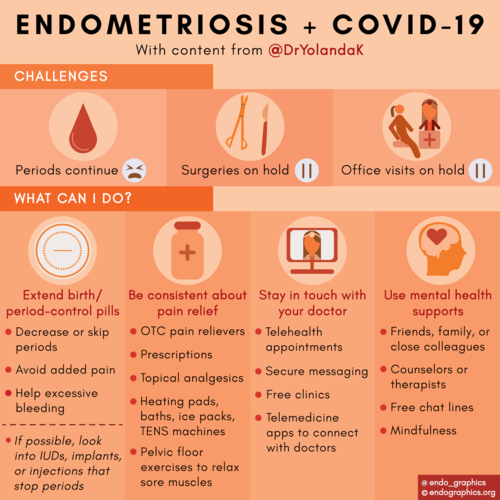
Infographic collaboration by Dr. Kirkham with endographics.org on treatment in the pandemic
The "Invisible Disease" of Endometriosis
Opinion by Dr. Yolanda Kirkham
TREATMENT
MEDICATION options (table 2)
Medical treatments (yourperiod.ca, SOGC)
Endometriosis diet (PDF) and detailed treatment info from BC Women’s Centre for Pelvic Pain & Endometriosis
Pain U self-help from TAPMI
Tamethebeast.org and MyCarePath Chronic pain resources
For those interested in advocating for Endometriosis Awareness and funding in Canada endoact.ca
Endometriosis
Endometriosis is a condition where tissue deposits similar to the lining of the uterus (endometrium) grow in the pelvis/abdomen. There are many theories about how endometriosis happens including older theories like backwards bleeding and newer theories like seeding, genetic, immune, cell changes. Endometriosis spots respond to your natural hormonal changes that go up and down with periods. Endometriosis causes inflammation because the body does not like blood, fluid, or other foreign tissue in this space. The deposits collect and get trapped in the cul-de-sacs in front of and behind the uterus (see diagram). Over time, the discomfort can worsen so that it happens even during times of the month when you’re not on your period. Endometriosis can also cause bladder and/or bowel symptoms because of the physical proximity and adhesions (“scarring” like sticky glue that attach the organs). Leg or back pains are common. Intercourse may also hurt. Often, moms, sisters, or aunts also had extremely painful periods.
Not everyone with endometriosis has all the symptoms. Not everyone has a lot of pain. Not everyone has difficulties getting pregnant, especially if treated early. Many people with endometriosis still have babies and especially if diagnosed and treated early. The amount of disease also does not correlate with the amount of pain. Ultrasound is often used to rule out other causes of pain. Endometriosis is not usually seen on ultrasound unless the disease is advanced or causing endometriomas (chocolate cysts in the ovary). That’s why many people end up leaving the emergency room with “normal” pelvic ultrasounds, unfortunately. Improvement in ultrasound techniques are being studied and utilized in different parts of the world. Loss of a “sliding sign” on ultrasound can suggest deeper infiltrative endometriosis. During laparoscopy surgery (which not everyone needs if medical treatment removes all pain and symptoms), endometriosis spots appear like paint splatter on the inner walls of your pelvis and abdomen. In young people, they can be pink or clear, like tapioca, and very subtle. All of the above factors make diagnosis difficult. But the pain is a big clue.
Surgery (laparoscopy) to excise (remove) endometriosis lesions can be helpful when medical treatment first does not improve the pain. But endometriosis is chronic and cannot be treated by surgery alone. Medication that leads to no more period bleeding is our first line of treatment (gets at the cause of pain). Postoperative hormonal suppression is also important to prevent recurrence of pain and disease unless immediately trying to conceive (pregnancy also leads to no periods and thus lack of endometriosis pain). There are many medical options but it may take some trial and error to find the right one for you. Because the pain is from microscopic bleeding and inflammation, treatment is to stop bleeding and to use anti-inflammatories when needed (take with food). Luckily, we now have lots of treatment options. Taking birth control pills/patch/vaginal ring back to back to skip periods, progestin injections/pills/IUD, or specialized medication for endometriosis are medication options. All of these medications thin the uterine lining so there is less or nil to bleed per month. Pain can be significantly reduced or eliminated, especially if diagnosed early, but there can be flares of pain and inflammation depending on your starting point. Anti-inflammatory pills, patches, creams from the drug store help for short flares. Even after surgery, medical treatment is still important to prevent regrowth of endometriosis (when periods continue) and recurrence of pain. A progestin IUD with the least amount of circulating hormones compared to pills, for example, can be inserted during surgery for 5 years continued treatment (leads to no periods). Lifestyle changes (exercise, nutrition, mindfulness), pelvic floor physiotherapy for pelvic floor relaxation (diaphragm belly breathing and cat/cow yoga positions, No kegels!), acupuncture, and additional measures are important to continue and sometimes pain may return. For those with chronic or return of pelvic pain, your doctor can also make a referral to a pain clinic which can be very helpful.
Diagram shows common locations of endometriosis deposits.