Period and Birth Control
Reproductive Health
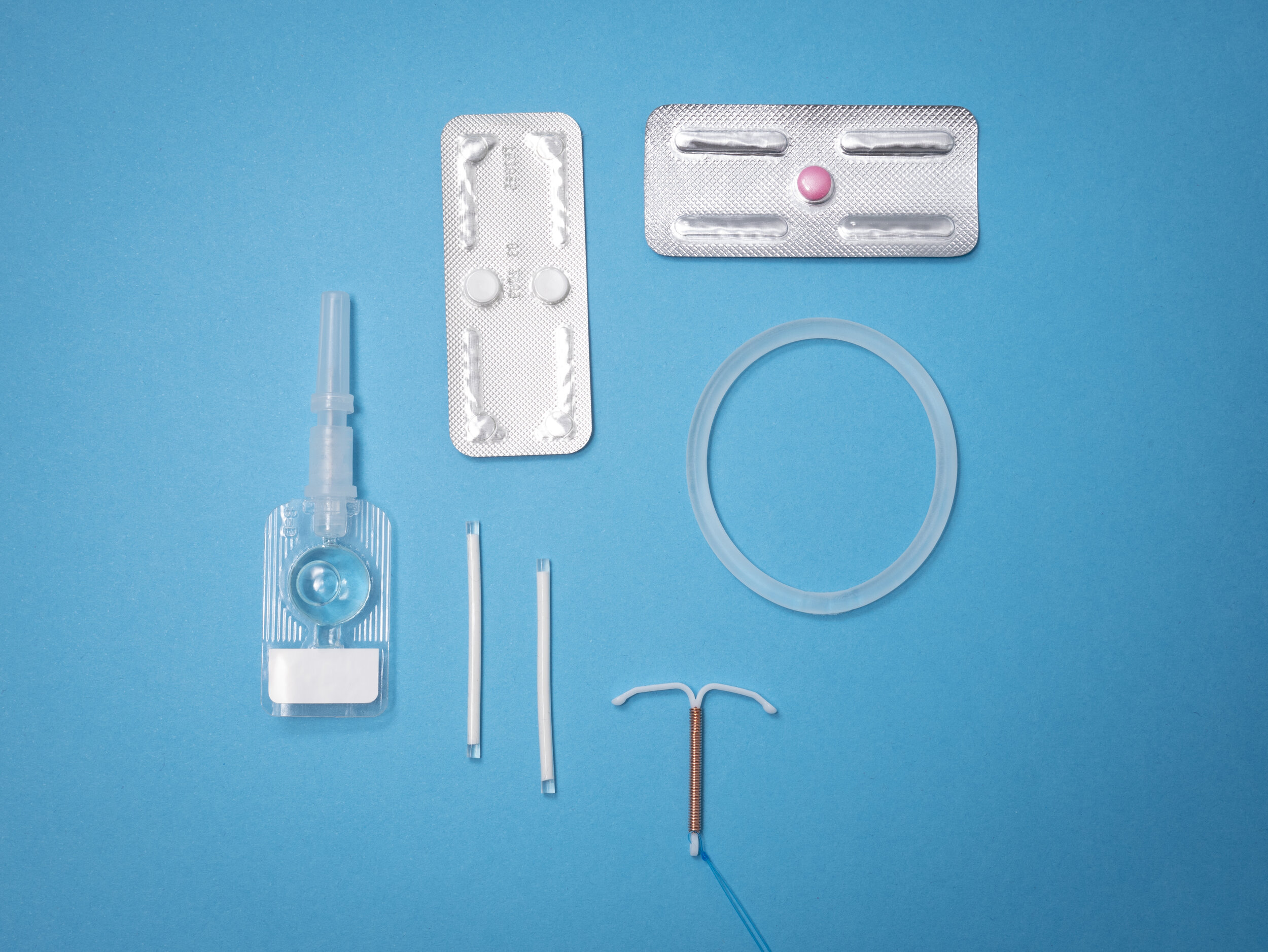
Contraceptive Options = Period Control Options
Every girl, woman, person is different and that is why there are so many options to choose from.
Pills, patches, rings, arm implants, progestin intrauterine devices (IUD), injections all help to manage period pain, flow, and regularity. They are also used to treat acne or PMS/PMDD.
Some people like pills, others prefer a “set it and forget it” (IUD) option.
Even if one didn’t work for you before, you could still find something else that is the right fit for you.
Most options have estrogen and progesterone, the hormones that regulate periods in your body.
Some are progesterone only (pill, arm implant, injection, intrauterine device IUD). These are safer for those with risks of age, leg or lung clots, smokers of more than 10 cigarettes per day. Progestin-based medicine to thin the uterus lining can also be more effective for those with endometriosis (estrogen-dependent) and prevents and reverses pre- or early uterine cancer.
Some have no hormones (copper IUD; contraception only, no period benefits).
None of the birth control methods protect against sexually transmitted infections. Only condoms do.
If someone has acne or PMS/PMDD (caused by body’s own fluctuating hormones) - systemic combined hormonal options work best (eg. pill, patch, ring) with no break so that doses remain the same daily.
If someone wants the least amount of circulating hormones but has heavy or painful periods, local progestin IUD (IUS) might work the best. They continuously thin the uterine lining so periods become very light or absent. They do not suppress ovulation so you would still have your own hormonal ups and downs. IUDs are now first-line for all ages. They are also used to reverse some pre-cancers (hyperplasia) of the uterus.
If someone has recurrent painful ruptured ovarian cysts or ovulation pain, pill/patch/ring would work the best to suppress ovulation (egg release = ovulation) as they simulate pregnancy.
The hormones thin the uterus lining so there is less to bleed each month. Usually, the uterus lining regenerates every month. Hormonal options can be used to skip periods altogether. And no, the lining does not build up because it’s thinned down by the progesterone (lawnmower hormone).
Some options are systemic (go into your bloodstream), others are more local (IUS) and may have fewer to no side effects. In fact, most people do not have any side effects.
Often, these medications are necessary in all age groups to
stop excessive bleeding
prevent blood transfusions or surgery
stop debilitating periods or endometriosis symptoms
prevent cancer (FACT: 5 -10 years of birth control pills, or IUD/IUS reduces uterus and ovary cancer risk by 50-80%. We actually use the progestin IUD to treat pre-cancer or hyperplasia of the uterus).
regulate periods, acne, mood due to hormonal imbalances (anovulatory cycles in PCOS, early teens, perimenopause).
Just as hormone regulation medications are used to correct thyroid, pancreas (diabetes), or brain (anxiety) conditions, we might sometimes need them to regulate period problems.
As with any medication, there can be risks and side effects. For pills/patch/ring that have estrogen, the risk of a blood clot in the leg or lung is 4-5 women in 10,000 for non-pill users; 9-10 in 10,000 for those on hormonal contraception with estrogen. These are lower risk than the clot risks in pregnancy: 30 in 10,000 for pregnant women (huge increase in hormones); 300-400 in 10,000 postpartum. Many people have no side effects; some have side effects that go away in a couple weeks; and for others they may persist on 1 type but have none or less effect on another. Rarely, use of pills/patch/ring for many years can be associated with vaginal or sex pain (vestibulodynia) in some patients. Thus, choosing the lowest dose options such as progestin IUD or copper IUD can be the best choice in these cases. Those on oral forms (minipill, dienogest), injections (depo), or arm implants with progestin-only should continue weight-bearing exercise and increase intake of foods with calcium and vitamin D to support their bones.
There are also non-hormonal options for decreasing flow and pains (anti-inflammatories) and medication (tranexamic acid) that work on the bleeding/clotting system taken only during heavy flow, but these do not usually address the underlying hormonal causes.
Table 3 in this National SOGC Guideline on Menstrual Suppression compares options.
Dr Kirkham explains in Flare Magazine 6 Myths about Birth Control, Debunked
Options and Failure Rates SOGC
What happens after you go off the pill? Today’s Parent
Choosing the right pill based on estrogenic, progestogenic, androgenic properties
Do we need to bleed monthly x 450? Are periods necessary?
Sexual and Reproductive Health
Sex & U Trusted resource from SOGC
What you need to know about getting a Pap test Best Health Magazine
HPV info.ca Reliable info about the vaccine that protects you from cervical, vulvar, vaginal cancer.
Rainbow Health Ontario LGBTQS2 info